Explore Moda Health’s medical, prescription, and dental plans – plus easy access to support and resources!
Salem Health is proud to partner with Moda Health for our medical plan coverage and prescription benefits.
You have a choice of two health plan options to cover yourself and your dependents. Each option provides comprehensive medical benefits, coverage for prescription drugs and free in-network preventive care. An in-network provider means a provider who is employed by Salem Health, West Valley Hospital or participating in Moda Health’s Connexus network.
You will always pay the least amount when you seek services from Salem Health providers and facilities. You may pay more for services when seeing a Connexus provider, but it is important to remember that you will always be protected from balance billing.
Prime Plan – High Deductible Plan (In-network coverage only, with a few exceptions)
Choice Plan – Medical Home Plan (In and Out-of-network coverage)
Not every plan is right for everyone, so review the details of each health plan option carefully. Consider the total cost of your health care benefit, including how much you pay upfront via payroll contributions compared to how much you pay at the time of service. Think also about how much you and your dependents use health care services and how much money you may need to save for future health care needs.
You will also need to understand your benefits and how your plan’s provider network impacts your coverage. The amount you will pay in copays (if applicable) and coinsurance (the percentage of cost share) will depend on the coverage Tier the provider you select falls under. It is a good idea to check your provider’s status at the start of each year to see what category they fall into.
Coverage Tiers
Both medical plans will cover the same types of medical services, but at different benefit levels (deductible, coinsurance and out-of-pockets will vary).
Tier I – Providers of Salem Health Hospitals & Clinics and facilities
- You will save the most on out-of-pocket expenses on both medical plans when you seek services from Salem Health providers and facilities
- Some specialists (including but not limited to pathologists, radiologists, dermatologists, gastroenterologists and bariatric surgeons) are not Salem Health employees or our affiliates’ staff, but are contracted specialists and are paid under Tier II or Ill. Not all services may have a Tier I provider.
- A listing of Salem Health medical providers accepting new patients can be viewed here: https://salemhealth.sharepoint.com/sites/SalemHealthMedicalGroup/SitePages/Open-Providers.aspx
Tier II – Moda’s Connexus network
- This network includes providers and clinics that generally provide services that are not available at Salem Health Hospitals & Clinics
- This includes, but is not limited to:
- Salem Clinic
- OHSU
- Legacy Emanuel and Randall Children’s Hospital
- Oregon Oncology Specialists
- Moda’s network of independent behavioral health and alternative care providers
- Moda’s network of providers that supply durable medical equipment
- Out-of-pocket expenses will be higher than if you choose a Tier I provider, but lower than if you choose a Tier III provider
Tier III – Moda’s Connexus network
- This includes specific hospital systems, ambulatory surgery centers and provider clinics that provide the same services as Salem Health Hospitals & Clinics
- For all in-network providers, out-of-pocket expenses will be the highest if you choose a Tier III provider
Tier IV – Providers that are not contracted by the Moda Health Connexus network and are considered out-of-network
- See below for a summary side by side view of all plans.
Travel and Out of Area Dependents
What are my medical benefits while traveling?
When traveling outside of the primary service area (Oregon/Southwest Washington), you can receive in-network, Tier II benefits by using a travel network provider for urgent or emergency services. Your travel network is the Aetna PPO network and you must seek care from an Aetna PPO provider to receive in-network coverage. The travel network can only be utilized if you are outside the primary service area and the travel is not for purposes of receiving treatment or benefits.
If you need help finding a provider, contact your Health Navigator team at 855‐425‐4543.
What is the coverage for dependents outside the primary service area?
Enrolled dependents residing in the United States, but outside the primary service area (Oregon/Southwest Washington), can receive care at the in-network, Tier II benefit level by using an Aetna PPO provider. When an enrolled dependent moves outside the primary service area, you must contact your Health Navigator team at 855‐425‐4543 to provide the dependent’s out-of-area address.
The dependent will be set up on an out-of-area plan and will be eligible for the out-of-area coverage the first day of the month following the notification to Moda.
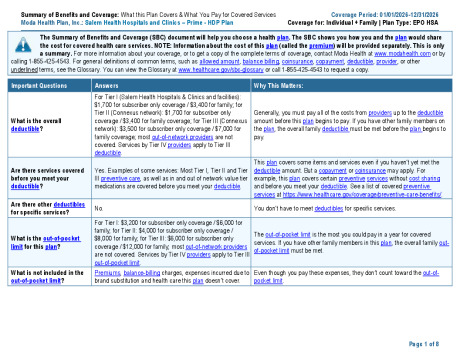
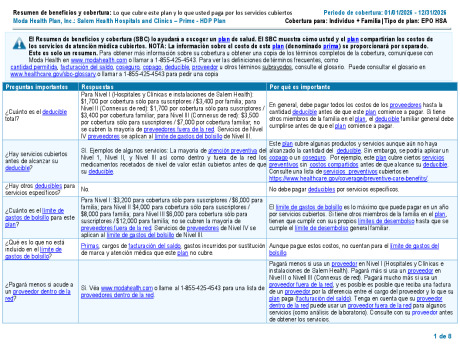
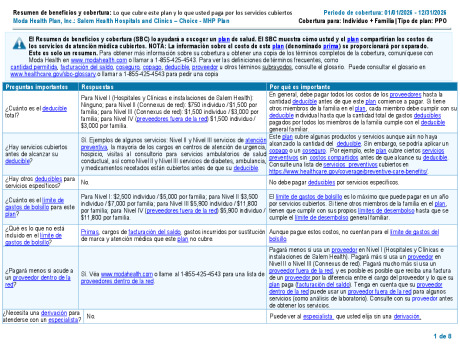
Prime Plan – HDP
Premium: $
Deductible: $$$
The Prime Plan – HDP provides comprehensive coverage and you can choose any in-network Tier I, Tier II, or Tier III physician or hospital for your care. Out-of-network coverage is limited to urgent and emergency care, massage therapy, acupuncture, spinal manipulation, and certain behavioral health services. Regardless of the provider you use, you generally pay co-insurance (a percentage) of eligible expenses once your deductible has been met.
The High Deductible Plan (HDP) gives you more control over your healthcare costs and is the only plan that features a Health Savings Account (HSA). Please see the Health Savings Account page for more information.
Key features of the HDP for you to consider:
- The HDP allows you to open a Health Savings Account (HSA). Pre-tax contributions can be made to your HSA to help pay the cost of the deductible and other eligible medical expenses. HSA’s can grow over time and rollover from year to year.
- You can enroll in a HSA and receive the employer contribution only if you are enrolled in the HDP.
- For eligible HSA participation, you (the employee) cannot be covered by any other medical plan, including Medicare, Tricare or a Health Flexible Spending Account unless that other coverage is also a qualified high deductible plan.
- View the Health Savings Account page for additional important HSA eligibility information.
- Your per-paycheck contributions are the lowest between the two plans.
- You can go to any in-network provider, but you’ll pay the least amount out of pocket when you go to Salem Health or West Valley Hospital. Applicable Tier 1 deductible must first be met.
- You are responsible for 100% of the cost of prescriptions until you meet your deductible – unless your medication is preventive (as defined by the Affordable Care Act) and therefore, the deductible is waived.
- You will be eligible to receive a employer contribution into a Health Savings Account:
o Up to $850 Employee Only or $1,700 Employee + Dependent(s). See the Health Savings Account page for important prorated contribution information.
o The HSA must be intentionally elected to be considered a participant and eligible for the employer contribution. A minimum of $.01 employee contribution is required.
o Employees must be active at work per the employer funding schedule chart to be eligible for the employer contribution.
o View the Health Savings Account page for additional important HSA eligibility information.
Medicare and Prime Plan - HDP
- If you or a covered dependent are Medicare eligible, or close to being Medicare eligible, speak with a Benefits Specialist to see how enrollment in the HDP might affect you.
- Review Salem Health’s Prime Plan – HDP Medicare Part D statement for important information regarding creditable prescription status.
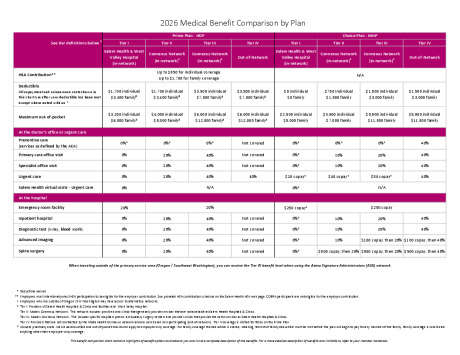
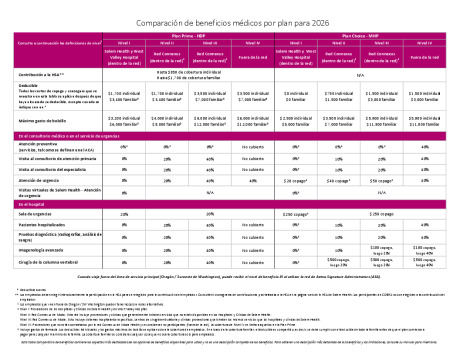
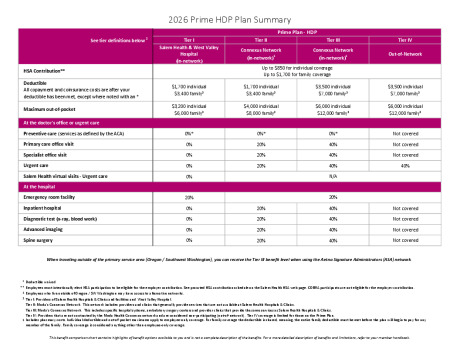
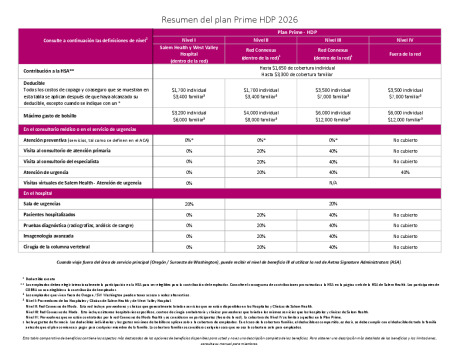
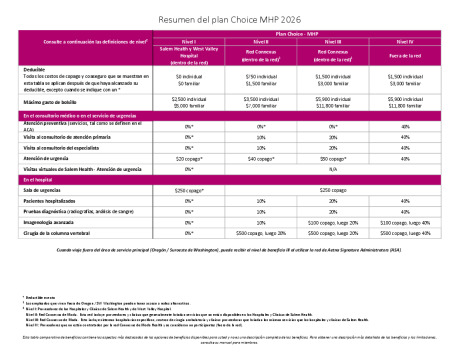
Prime Plan - HDP Summary Grid
Important note: The deductible must be met before the plan will begin to pay for any services (other than preventive care) and this includes prescription expenses as well. For employees with family coverage, meaning you have dependents enrolled on the plan, the entire family deductible must be met before the plan will begin to pay for any member of the family.
| Prime Plan - HDP See Tier definitions below ³ |
Tier I Salem Health & West Valley Hospital (in-network) |
Tier II Connexus Network (in-network)2 |
Tier III Connexus Network (in-network)2 |
Tier IV Out-of-Network |
||||
|---|---|---|---|---|---|---|---|---|
| HSA Contribution | $850 individual coverage $1,700 family coverage |
|||||||
| Deductible | $1,700 individual $3,400 family |
$1,700 individual $3,400 family |
$3,500 individual $7,000 family |
$3,500 individual $7,000 family | ||||
| Maximum out-of-pocket | $3,200 individual $6,000 family |
$4,000 individual $8,000 family |
$6,000 individual $12,000 family |
$6,000 individual $12,000 family | ||||
| At the doctor's office or urgent care | ||||||||
|
Preventive care (services as defined by the ACA) |
0%* | 0%* | 0%* | Not covered | ||||
| Primary care office visit | 0% | 20% | 40% | Not covered | ||||
| Specialist office visit | 0% | 20% | 40% | Not covered | ||||
| Urgent care | 0% | 20% | 40% | 40% | ||||
| Salem Health virtual visits - Urgent care |
0% | N/A | ||||||
| At the hospital | ||||||||
| Emergency room facility | 20% | |||||||
| Inpatient hospital | 0% | 20% | 40% | Not covered | ||||
|
Diagnostic test (blood work) |
0%3 | 20% | 40% | Not covered | ||||
| Advanced imaging | 0%3 | 20% | 40% | Not covered | ||||
| Spine surgery | 0% | 20% | 40% | Not covered | ||||
| Other medical benefits | ||||||||
|
Outpatient rehabilitation (physical, occupational or speech therapies)1 |
0% | 20% | 40% | Not covered | ||||
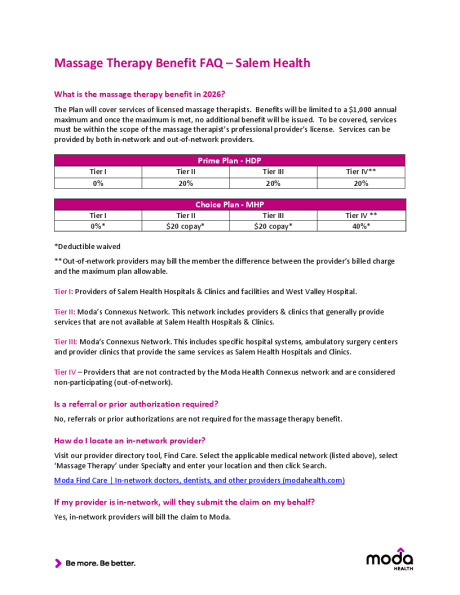
| Massage therapy1 | 0% | 20% | 20% | 20% | ||||
| Acupuncture11 | 0% | 20% | 20% | 20% | ||||
| Spinal manipulation1 | 0% | 20% | 20% | 20% | ||||
| Sleep studies | 0% | 20% | 40% | Not covered | ||||
| Upper endoscopy | 0% | 20% | 40% | Not covered | ||||
| Mental Health and Substance Use Disorder | ||||||||
| Outpatient mental health & substance use disorder office visits | 0% | 0% | 0% | 0% | ||||
| Residential mental health & substance use disorder treatment programs | 0% | 0% | 0% | 40% | ||||
| Substance use disorder detoxification | 0% | 20% | 20% | 40% | ||||
* Deductible waived
1 Limitations apply
2 Employees who live outside of Oregon / SW Washington may have access to alternative networks
3 Tier I: Providers of Salem Health Hospitals & Clinics and facilities. Tier I benefits apply to services billed by Salem Health Medical Group and Salem Health facilities. Some specialists (e.g. pathologists and radiologists) are not Salem Health employees or our affiliates’ staff, but are contracted specialists and are paid under Tier II or Ill. Not all services may have a Tier I provider.
Tier II: Moda’s Connexus Network. This network includes providers & clinics that generally provide services that are not available at Salem Health Hospitals & Clinics.
Tier III: Moda’s Connexus Network. This includes specific hospital systems, ambulatory surgery centers and provider clinics that provide the same services as Salem Health Hospitals and Clinics
Tier IV – Providers that are not contracted by the Moda Health Connexus network and are considered non‐participating (out‐of‐network). Tier IV coverage is limited for those on the Prime Plans.
This benefit comparison chart contains highlights of benefit options available to you and is not a complete description of the benefits. For a more detailed description of benefits and limitations, refer to your member handbook.
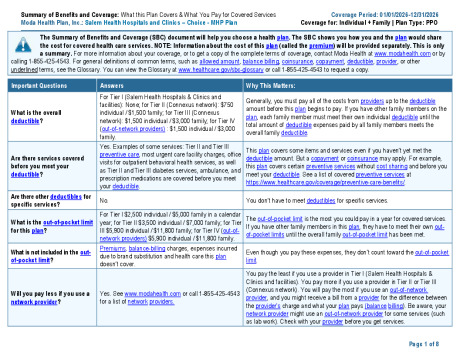
Choice Plan – MHP
Premium: $$$
Deductible: $
- Your per-paycheck contributions will be the highest of the two plans, but you will have a lower deductible and out-of-pocket maximum
- You can go to any provider, but you’ll pay the least when you go to Salem Health or West Valley Hospital.
- You have coverage with out-of-network providers, however, you may be balanced billed for services.
- You are not eligible for the Health Savings Account.
- You are eligible to participate in the Healthcare Flexible Spending Account.
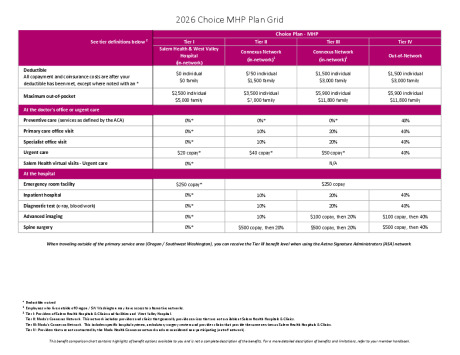
Choice Plan - MHP Summary Grid
| Choice Plan - MHP See Tier definitions below ³ |
Tier I Salem Health & West Valley Hospital (in-network) |
Tier II Connexus Network (in-network)2 |
Tier III Connexus Network (in-network)2 |
Tier IV Out-of-Network |
||||
|---|---|---|---|---|---|---|---|---|
| HSA Contribution | N/A | |||||||
| Deductible | $0 individual $0 family |
$750 individual $1,500 family |
$1,500 individual $3,000 family |
$1,500 individual $3,000 family | ||||
| Maximum out-of-pocket | $2,500 individual $5,000 family |
$3,500 individual $7,000 family |
$5,900 individual $11,800 family |
$5,900 individual $11,800 family | ||||
| At the doctor's office or urgent care | ||||||||
|
Preventive care (services as defined by the ACA) |
0% | 0%* | 0%* | 40% | ||||
| Primary care office visit | 0% | 10% | 20% | 40% | ||||
| Specialist office visit | 0% | 10% | 20% | 40% | ||||
| Urgent care | $20 copay | $40 copay* | $50 copay* | 40% | ||||
| Salem Health virtual visits - Urgent care |
0% | N/A | ||||||
| At the hospital | ||||||||
| Emergency room facility | $250 copay | |||||||
| Inpatient hospital | 0% | 10% | 20% | 40% | ||||
|
Diagnostic test (blood work) |
0%3 | 10% | 20% | 40% | ||||
| Advanced imaging | 0%3 | 10% | $100 copay, then 20% | $100 copay, then 40% | ||||
| Spine surgery | 0% | $500 copay, then 20% | $500 copay, then 20% | $500 copay, then 40% | ||||
| Other medical benefits | ||||||||
|
Outpatient rehabilitation (physical, occupational or speech therapies)1 |
0% | 10% | 20% | 40% | ||||
| Massage therapy1 | 0% | $20 copay* | $20 copay* | 40%* | ||||
| Acupuncture1 | 0% | $20 copay* | $20 copay* | 40%* | ||||
| Spinal manipulation1 | 0% | $20 copay* | $20 copay* | 40%* | ||||
| Sleep studies | 0% | $100 copay, then 20% | $100 copay, then 20% | $100 copay, then 40% | ||||
| Upper endoscopy | 0% | $100 copay, then 20% | $100 copay, then 20% | $100 copay, then 40% | ||||
| Mental Health and Substance Use Disorder | ||||||||
| Outpatient mental health & substance use disorder office visits | 0% | $0* | $0* | $0* | ||||
| Residential mental health & substance use disorder treatment programs | 0% | 0%* | 0%* | 40% | ||||
| Substance use disorder detoxification | 0% | 10% | 10% | 40% | ||||
* Deductible waived
1 Limitations apply
2 Employees who live outside of Oregon / SW Washington may have access to alternative networks
3 Tier I: Providers of Salem Health Hospitals & Clinics and facilities. Tier I benefits apply to services billed by Salem Health Medical Group and Salem Health facilities. Some specialists (e.g. pathologists and radiologists) are not Salem Health employees or our affiliates’ staff, but are contracted specialists and are paid under Tier II or Ill. Not all services may have a Tier I provider.
Tier II: Moda’s Connexus Network. This network includes providers & clinics that generally provide services that are not available at Salem Health Hospitals & Clinics.
Tier III: Moda’s Connexus Network. This includes specific hospital systems, ambulatory surgery centers and provider clinics that provide the same services as Salem Health Hospitals and Clinics
Tier IV – Providers that are not contracted by the Moda Health Connexus network and are considered non‐participating (out‐of‐network). Tier IV coverage is limited for those on the Classic and Prime Plans.
This benefit comparison chart contains highlights of benefit options available to you and is not a complete description of the benefits. For a more detailed description of benefits and limitations, refer to your member handbook.